After decades of stigma and prohibition, psychedelic substances are experiencing a renaissance in medical research and mental health treatment. A growing body of rigorous scientific studies and clinical trials published in some of the world’s top medical journals is legitimizing psychedelics as promising treatments for some of the most challenging psychiatric conditions, including post-traumatic stress disorder (PTSD), depression, and addiction. This exciting revival blends ancient spiritual traditions with modern neuroscience, giving hope to millions of patients for whom conventional therapies have failed.
Psychedelics: A Modern Renaissance Rooted in Tradition and Science
The renewed interest in psychedelics such as psilocybin (magic mushrooms), lysergic acid diethylamide (LSD), and 3,4-methylenedioxymethamphetamine (MDMA) is driven by transformative research that combines decades of anecdotal evidence, shifting cultural attitudes, and breakthroughs in brain imaging. These substances modulate consciousness and perception in ways that can promote profound psychological insight, emotional breakthroughs, and neural plasticity.
Historically, psychedelics were used ritually by many indigenous cultures worldwide, but Western society relegated them to controlled substances after the political backlash of the 1960s. Today’s psychedelic medicine integrates this rich cultural heritage with stringent scientific protocols to ensure safety, efficacy, and therapeutic efficacy.
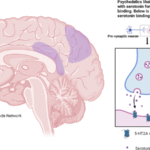
The Neurobiology of Psychedelics: Hacking the Brain to Promote Healing
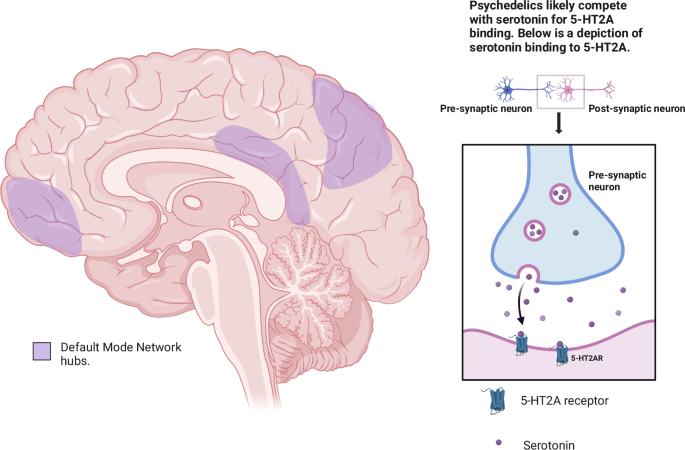
Recent studies provide insight into how psychedelics alter brain activity and promote lasting therapeutic benefits. Neuroimaging studies of healthy volunteers given high doses of psilocybin show disruption of the default mode network (DMN), a brain network associated with self-referential thinking and the sense of ego. This “desynchronization” reduces habitual, rigid patterns of thought associated with depression and other disorders, temporarily “quieting” the overactive brain systems that sustain pathological states.
Crucially, psilocybin produces a lasting “reset” effect on connectivity between the hippocampus (involved in memory) and the DMN, creating enhanced neural plasticity that persists for months afterward. This heightened plasticity allows patients to better engage with psychotherapy and reprocess traumatic memories or depressive thought patterns.
Dr. Joshua Siegel, a neuroscientist and lead author on this research, explained:
“Putting these parts of the brain into a more plastic and adaptable state seems to help people change behavior. When therapy is used in this setting, it allows people to take advantage of this increased flexibility to overcome maladaptive patterns.”
Psychedelic-Assisted Therapy (PAT) for PTSD
PTSD, a debilitating condition caused by trauma, has shown particular promise in response to psychedelic-assisted therapy (PAT). While MDMA-assisted psychotherapy has attracted much attention recently, other psychedelics like psilocybin and ketamine are being examined with growing interest.
An open-label pilot study at Ohio State University combining psychedelics with psychotherapy for treatment-resistant PTSD found statistically significant reductions in PTSD symptoms one month after treatment. Veterans using ibogaine and 5-MeO-DMT in clinical programs have reported substantial improvements in PTSD symptoms and suicidal ideation. Though research is early-stage, expert consensus believes that psychedelics facilitate the processing of traumatic material and promote emotional healing in ways that conventional therapies struggle to achieve.
Psychedelic sessions typically involve:
- Preparation sessions to set expectations and establish trust
- Guided dosing sessions where patients experience altered states
- Integration sessions to process insights and reinforce new perspectives
Protocols often include six or more 60-90 minute therapy sessions combined with one or two extended psychedelic experiences lasting several hours.
Clinical Evidence for Depression and Anxiety
Depression, particularly treatment-resistant forms, is another condition where psychedelics have shown remarkable promise. Randomized controlled trials with psilocybin have documented significant and sustained reductions in depressive symptoms, with effects lasting months after one or two treatment sessions.
A recent trial conducted on clinicians experiencing depression amid the COVID-19 pandemic demonstrated that psilocybin therapy resulted in a mean decrease of depressive symptoms scores by nearly 60% at 28 days post-treatment, significantly outperforming placebo controls.
Meta-analyses also suggest that psychedelic-assisted therapy yields large reductions in anxiety and depressive symptoms compared to both placebo and standard treatments. These improvements are thought to be mediated through enhanced neuroplasticity, altered brain network connectivity, and effective psychotherapy integration during the “window of brain plasticity”.
Psychedelics for Addiction Treatment
Traditional addiction treatments have often struggled with high relapse rates and limited efficacy. Psychedelic-assisted therapy offers novel mechanisms for disrupting addictive patterns and fostering enduring recovery.
Clinical evidence indicates that substances like psilocybin, LSD, and ibogaine improve abstinence rates and reduce cravings in patients addicted to alcohol, nicotine, and opioids. For example, psilocybin-assisted smoking cessation treatment shows one-year abstinence rates approaching 60%, exceeding those of conventional therapies.
MDMA-assisted therapy is under investigation for treating substance use disorders, and preliminary results indicate reductions in substance use and improvements in mental health symptoms. Psychedelics may facilitate emotional breakthroughs, reduce avoidance, and enhance motivation for behavioral change, complementing psychotherapeutic support.
Mechanisms Underpinning Psychedelic Effects on Mental Health
Clinical and preclinical research suggests multiple neurobiological mechanisms through which psychedelics exert therapeutic effects:
- Neural Plasticity: Psychedelics increase synaptogenesis and dendritic growth, helping repair neural circuits disrupted by trauma or chronic depression.
- Network Reorganization: Temporary disruption of rigid brain networks like the DMN promotes cognitive flexibility and new perspectives.
- Emotional Processing: Psychedelics can dampen fear-based responses in the amygdala, facilitating trauma processing and emotional release.
- Heightened Suggestibility: The heightened suggestibility during psychedelic experiences enhances psychotherapy efficacy, allowing patients to reframe and integrate difficult emotional material.
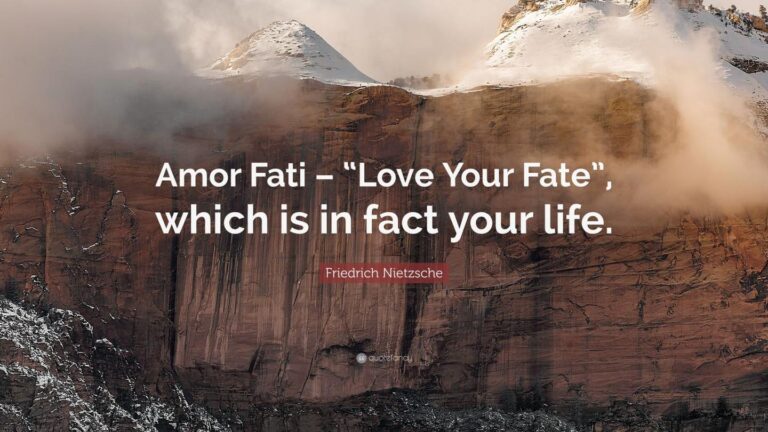
- Spiritual and Mystical Experiences: Many patients report transformative spiritual or mystical-like experiences that promote meaning, connectedness, and psychological well-being.
Safety, Risks, and Ethical Considerations
Psychedelics demonstrate a reassuring safety profile when administered within controlled clinical contexts with medical monitoring. Serious adverse events are rare but possible, particularly in patients with psychotic disorders or certain cardiovascular conditions.
Psychological distress during experiences (e.g., anxiety or panic) can occur but is usually transient and managed with skilled therapeutic support. The slow and careful dosing combined with pre-screening and integration is essential to minimize risks.
Ethical delivery also requires culturally competent care, informed consent, and ongoing research to understand long-term effects fully.
Legal Status and the Path to Mainstream Medicine
Several psychedelic compounds have received “breakthrough therapy” designations from the FDA for depression and PTSD treatment, expediting clinical development.
Psilocybin and MDMA are closest to potential approval and introduction into medical practice, with phase 3 trials underway.
Despite legalization advances at the state and city levels, federal law in the U.S. still prohibits most psychedelics, complicating access and research. The coming years are likely to see efforts to harmonize legal reforms with evidence-based medical use.
Future Directions and Challenges
Ongoing challenges for psychedelic medicine include:
- Scale-up of trained therapists and clinical frameworks
- Insurance coverage and affordability
- Addressing stigma and public misconceptions
- Balancing commercialization with equity and ethical concerns
- Conducting large-scale longitudinal studies to assess durability of effects and identify responders and non-responders.
Importantly, continued research into neuropsychopharmacology and brain imaging promises to unravel more precise mechanisms, fostering tailored interventions for diverse mental health conditions.
Conclusion: A Hopeful New Paradigm for Mental Health
The renaissance of psychedelics marks a profound shift in mental health treatment—moving beyond symptom suppression toward holistic healing that addresses the root causes of suffering. Scientific evidence confirms that substances like psilocybin, MDMA, and LSD can offer durable benefits for conditions such as treatment-resistant depression, PTSD, and addiction when paired with skilled psychotherapy.
The neuroplastic and transformative effects of psychedelics open new avenues for emotional healing, integration of trauma, and restoration of meaning and connection. While challenges remain in safely scaling and regulating these powerful therapies, the momentum of rigorous research and growing cultural acceptance signals a hopeful future where psychedelics reclaim their role as catalysts for mental health and well-being.
As research progresses, psychedelics may soon become mainstream tools in psychiatric medicine—ushering a longer, deeper “trip” toward recovery, self-discovery, and human flourishing.
References
- Global Wellness Institute, „Psychedelics & Healing Initiative Trends for 2025“
- Siegel, J. S. et al., Nature, 2024 — psilocybin neuroimaging study
- American Psychological Association Monitor, „Psychedelic treatment and mental health“, 2025
- PubMed, Psychedelics for the Treatment of Psychiatric Disorders, 2025
- McLean Hospital, Exploring Psychedelic-Assisted Therapy, 2024
- Lisbon Addictions Europe, Psychedelic Therapy in Addiction, 2024
- PTSD National Center for PTSD, Psychedelic-Assisted Therapy for PTSD, 2024