This in-depth exploration unpacks the human body’s natural opioid system—shedding light on how endogenous opioids like endorphins are synthesized, how they bind to receptors, and how these mechanisms influence pain, pleasure, and emotional regulation. The post delves into the neurobiology of opioid receptors (mu, delta, and kappa), their role in reward pathways, and how external opioids hijack these systems to create dependency. Drawing from cutting-edge research, it also examines the genetic, psychological, and environmental roots of opioid addiction, offering insights into treatment strategies and the future of pain management. Whether you’re a healthcare professional, psychology enthusiast, or someone seeking clarity on addiction science, this blog offers a clear, compassionate, and scientifically grounded guide.
Understanding Your Body’s Built-In Pain Relief System
Your body has its own natural pharmacy that produces pain-relieving chemicals called endogenous opioids. These are your body’s version of morphine—substances that can make you feel better when you’re hurt, stressed, or need comfort. The word “endorphin” actually comes from combining “endogenous” (made inside your body) and “morphine”.
Your Body Makes Three Types of Natural Opioids
Think of your body as having three different factories that produce pain relief:
The Beta-Endorphin Factory is mainly located in your pituitary gland (a small gland at the base of your brain). This factory starts with a large protein called POMC and cuts it into smaller pieces, one of which becomes beta-endorphin—your body’s most powerful natural painkiller. This process happens when your brain detects stress, pain, or intense physical activity.
The Enkephalin Factory is spread throughout your brain and spinal cord. It produces two main products: Met-enkephalin and Leu-enkephalin—small proteins that help manage pain locally where they’re made. These work like a neighborhood pain relief system, providing help right where it’s needed.
The Dynorphin Factory is primarily in your hypothalamus (a brain region that controls basic functions). Unlike the other two, dynorphins can travel long distances through your brain to provide pain relief in areas far from where they’re made.
How These Natural Painkillers Work
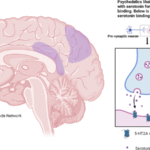
Your natural opioids work by attaching to special receptors throughout your nervous system—like keys fitting into locks. There are three main types of these locks:
- Mu receptors are the most important for both pain relief and addiction
- Delta receptors help with emotions and mood
- Kappa receptors are involved in stress responses
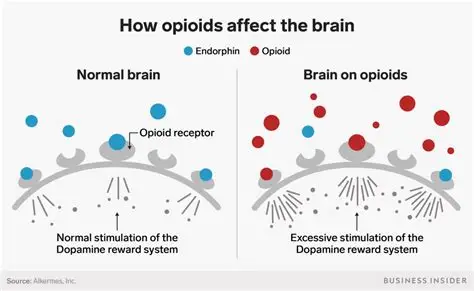
When your natural opioids attach to these receptors, they tell your nerve cells to calm down and stop sending pain signals. In your spinal cord, they block the release of substance P, a chemical that carries pain messages to your brain. In your brain, they work differently—they reduce the activity of inhibitory neurons, which allows more dopamine (the “feel-good” chemical) to be released.
How External Opioids Hijack Your Brain’s Reward System
The Dopamine Highway
Your brain has a built-in reward system designed to make you feel good when you do things that help you survive—like eating when hungry or finding safety when threatened. This system works through a “highway” of nerve cells that release dopamine, creating feelings of pleasure and satisfaction.
Here’s how it normally works:
- Your brain recognizes something rewarding (like food when you’re hungry)
- Nerve cells in the ventral tegmental area (VTA) get activated
- These cells release dopamine along the “highway” to the nucleus accumbens
- This dopamine release makes you feel good and want to repeat the behavior
Why Opioids Are Different
External opioids (like prescription painkillers or heroin) hijack this system in a uniquely powerful way. Instead of just activating the reward system directly, they work by removing the brain’s natural “brakes.”
Your brain normally has GABA neurons that act like brakes on dopamine release, preventing you from feeling too good all the time. Opioids attach to receptors on these brake neurons and shut them off. With the brakes removed, dopamine neurons fire much more than they normally would—sometimes 10 times more than with natural rewards.
This creates an intensely pleasurable experience that far exceeds anything your body can naturally produce. It’s like comparing the light from a candle to the light from a floodlight—both provide light, but one is overwhelmingly brighter.
Why Opioids Are More Addictive Than Other Drugs
The Perfect Storm for Addiction
Opioids create addiction through multiple mechanisms working together:
Tolerance develops quickly: Your brain tries to maintain balance, so when opioids repeatedly remove the “brakes” from dopamine neurons, your brain responds by making those brakes stronger and more numerous. This means you need increasingly larger amounts of opioids to get the same effect.
Physical dependence is inevitable: Unlike many other drugs, anyone who takes opioids regularly for more than a few weeks will develop physical dependence. This happens because your brain chemistry adapts to expect the opioids to be present.
Dual reinforcement: Opioids provide both positive reinforcement (making you feel extremely good) and negative reinforcement (taking them away makes you feel terrible). This creates a psychological trap where the drug becomes the solution to the problem it created.
How Your Brain Changes
With repeated opioid use, your brain undergoes profound changes that persist long after the drugs leave your system:
The reward system becomes broken: Normal pleasures like food, friendship, or accomplishments no longer feel rewarding because your dopamine system has been damaged. Only opioids can still activate this damaged system effectively.
The stress system becomes hyperactive: Areas of your brain that process stress and negative emotions become overactive, creating persistent anxiety, depression, and emotional distress.
Decision-making areas are impaired: The prefrontal cortex—responsible for good judgment and impulse control—becomes less active, making it harder to make rational decisions about drug use.
The Withdrawal Experience: Why It’s So Hard to Stop
What Withdrawal Feels Like
Opioid withdrawal creates a combination of physical and psychological symptoms that can be overwhelming:
Early symptoms (6-12 hours after last use):
- Intense anxiety and restlessness
- Muscle aches and pains
- Runny nose and tearing eyes
- Trouble sleeping
- Yawning and sweating
Peak symptoms (1-3 days):
- Severe nausea and vomiting
- Diarrhea and stomach cramps
- Dilated pupils and sensitivity to light
- Racing heart and high blood pressure
- Intense drug cravings
- Severe depression and hopelessness
Why Withdrawal Is So Severe
The severity of opioid withdrawal stems from how extensively these drugs affect your nervous system:
Your stress system goes into overdrive: A brain region called the locus coeruleus, which normally regulates alertness and stress responses, becomes hyperactive when opioids are removed. This creates intense physical discomfort and anxiety.
Your pain sensitivity increases: Without opioids blocking pain signals, you become extremely sensitive to any discomfort. Normal sensations become painful, and actual pain becomes unbearable.
Your mood regulation fails: The brain chemicals responsible for mood become severely imbalanced, creating depression, anxiety, and emotional instability that can last for months.
Timeline and Recovery
The acute withdrawal phase follows predictable patterns:
- Short-acting opioids (heroin, immediate-release pills): Symptoms start within 6-12 hours, peak at 1-3 days, and improve within a week
- Long-acting opioids (methadone, extended-release pills): Symptoms start within 24-36 hours, peak later, and can last 2-3 weeks or more
However, many people experience protracted withdrawal syndrome—subtle but persistent symptoms including sleep problems, anxiety, depression, and intense cravings that can last months or even years. This extended recovery period helps explain why relapse rates are so high.
Physical Dependence vs. Addiction: Understanding the Difference
It’s crucial to understand that physical dependence and addiction are not the same thing, though they often occur together:
Physical dependence is a predictable biological response that occurs in virtually anyone who takes opioids regularly, including patients legitimately prescribed them for pain management. It simply means your body has adapted to the presence of the drug and will experience withdrawal if it’s stopped suddenly.
Addiction (opioid use disorder) is a chronic brain disease characterized by compulsive drug-seeking behavior despite harmful consequences. It involves changes in brain circuits related to reward, stress, and self-control that persist long after drug use stops.
Only about 8% of patients prescribed opioids for legitimate pain management develop addiction, while nearly 100% develop some degree of physical dependence. This distinction is important for reducing stigma and ensuring appropriate medical care.
Why Opioids Are Harder to Quit Than Almost Any Other Substance
Unique Neurobiological Challenges
Several factors make opioid cessation particularly difficult compared to other addictive substances:
Severe physical withdrawal syndrome: While many drugs cause psychological withdrawal, opioids create intense physical symptoms that last for weeks. The immediate relief that opioid use provides for these symptoms creates powerful motivation to continue using.
Kindling effect: Each cycle of opioid use and withdrawal appears to make the brain’s stress systems more sensitive, making subsequent withdrawal episodes progressively more severe and difficult to endure.
Hijacked survival mechanisms: Opioids activate the same brain circuits that evolved to ensure survival behaviors like finding food and avoiding danger. When these circuits associate opioids with survival, quitting feels as impossible as stopping breathing.
Long-lasting brain changes: The structural and chemical changes in the brain from chronic opioid use can persist for months or years, creating vulnerability to relapse long after the acute withdrawal phase passes.
Individual Risk Factors
Some people are particularly vulnerable to opioid addiction due to:
- Genetic predisposition: Approximately 40-60% of addiction risk appears to be inherited
- Mental health conditions: Depression, anxiety, PTSD, and trauma history increase vulnerability
- Stress system dysfunction: People with altered stress responses show heightened addiction risk
- Early exposure: Younger brains are more susceptible to addiction-related changes
Hope for Recovery
Despite these challenges, recovery from opioid addiction is possible with appropriate treatment and support. Understanding the neurobiological basis of addiction helps explain why willpower alone is rarely sufficient—the brain changes that drive continued use require medical intervention and long-term support to overcome.
Medications like methadone, buprenorphine, and naltrexone can help normalize brain chemistry while behavioral therapies address learned patterns of drug use. Most importantly, recognizing addiction as a medical condition rather than a moral failing reduces stigma and encourages people to seek the help they need.
The complex mechanisms by which opioids affect the brain—from mimicking and overwhelming our natural opioid systems to creating lasting changes in reward and stress circuits—explain why these substances pose such extraordinary risks for addiction. With proper understanding and treatment, however, people can recover and reclaim their lives from opioid dependence.
Sources:
- What is the timeline for opioid withdrawal?
- The Neurobiology of Opioid Dependence: Implications for Treatment
- Neuroplasticity of the extended amygdala in opioid withdrawal and prolonged opioid abstinence
- Brain Reward System
- How opiod disorder occur
- Biochemistry, Endorphin
- Five Decades of Research on Opioid Peptides: Current Knowledge and Unanswered Questions
- Opiod receptors