Beyond immediate psychological distress, chronic anxiety in corporate offices and colleges exacts a profound physical toll—driving cardiovascular disease, gastrointestinal disorders, weakened immunity, chronic pain, and metabolic dysfunction. Addressing anxiety’s root causes and investing in holistic wellbeing programs are vital to safeguarding both mental and physical health.
Introduction
Anxiety—once perceived as a purely mental health concern—now reveals its far-reaching impact on the body. As corporate employees and college students grapple with relentless multitasking, incessant digital demands, and high-stakes performance pressures, the rising prevalence of anxiety is precipitating long-term physical illnesses. This blog delves into how chronic stress translates into chronic disease, examines the mechanisms at play, and proposes comprehensive strategies to mitigate these aftereffects.
The Anatomy of Stress: From Mind to Body
The Stress Response and Allostatic Load
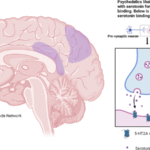
When individuals perceive stress—whether from looming deadlines or back-to-back exams—the body activates the hypothalamic–pituitary–adrenal (HPA) axis, releasing cortisol and adrenaline. Short bursts of these hormones are adaptive; however, sustained activation leads to “allostatic load,” a wear-and-tear process that chronically dysregulates multiple organ systems. Over time, elevated cortisol impairs cardiovascular health, suppresses immune function, disrupts metabolic regulation, and alters pain perception. For more on allostatic load, see the American Psychological Association’s overview.
Cardiovascular Consequences
Hypertension and Heart Disease
- Elevated Blood Pressure: Chronic anxiety correlates with persistently raised blood pressure. Meta-analytic evidence shows that individuals with generalized anxiety disorder have a 26% higher risk of hypertension than non-anxious peers.
- Increased Cardiovascular Events: Longitudinal studies link high anxiety scores to a 60% greater risk of heart attack and stroke over 10 years.
Mechanism: Cortisol-induced sodium retention, vascular inflammation, and endothelial dysfunction accelerate atherosclerosis, while sympathetic overdrive increases heart rate and cardiac workload. For clinical guidelines, refer to the American Heart Association’s recommendations on stress management.
Gastrointestinal Disorders
Irritable Bowel Syndrome (IBS) and Peptic Ulcers
- IBS Prevalence: Approximately 40% of patients with IBS report coexisting anxiety disorders. Chronic stress alters gut motility and permeability, fostering visceral hypersensitivity and dysbiosis.
- Ulcer Risk: Elevated cortisol exacerbates gastric acid secretion, impairing mucosal defenses. Anxiety-prone individuals exhibit twice the incidence of peptic ulcers.
Brain–gut axis signaling via the enteric nervous system amplifies discomfort, pain, and digestive irregularities. Explore the gut–brain connection in the National Institute of Diabetes and Digestive and Kidney Diseases fact sheet.
Immune Disregulation and Susceptibility to Illness
Increased Infections and Autoimmunity
- Weakened Immunity: Chronically high cortisol and catecholamines suppress lymphocyte proliferation, reduce natural killer (NK) cell activity, and impair antibody responses. Anxious individuals report 25% more frequent colds and flu.
- Autoimmune Flare-Ups: Dysregulated immunity can trigger or worsen conditions—such as rheumatoid arthritis and lupus—through proinflammatory cytokine overproduction. For detailed research, see the National Institutes of Health paper on stress and immunity.
Chronic Pain and Musculoskeletal Strain
Headaches, Back Pain, and Fibromyalgia
- Tension Headaches: Up to 75% of chronic headache sufferers report anxiety as a key trigger. Peripheral muscle tension and central sensitization heighten pain perception.
- Lower Back Pain: Workplace multitasking often involves prolonged static postures under stress, increasing risk of chronic back pain by 30%.
- Fibromyalgia Risk: Anxiety and stress-induced central nervous system sensitization contribute to widespread musculoskeletal pain syndromes. The Mayo Clinic’s overview of fibromyalgia offers further reading.
Metabolic and Endocrine Effects
Weight Disregulation and Diabetes
- Abdominal Obesity: Cortisol promotes visceral fat deposition. Anxious individuals have a 35% higher likelihoodof metabolic syndrome, a precursor to type 2 diabetes.
- Insulin Resistance: Chronic stress impairs insulin sensitivity; over time, this elevates fasting glucose and hemoglobin A1c levels, doubling diabetes risk. The International Diabetes Federation provides guidelines on metabolic syndrome.
Anxiety’s Long-Term Impact in Corporate Offices
Workplace Stress Exacerbates Physical Illness
- Absenteeism and Presenteeism: Chronic health conditions lead to 12.7% more sick days per year, and impaired productivity when present at work.
- Healthcare Costs: Employers face 42% higher healthcare expenditures for employees with anxiety-related chronic diseases.
Case Study: A multinational tech firm found that employees scoring above the clinical threshold for anxiety had medical claims averaging $3,200 annually—$1,000 more than lower-stress colleagues. For policies on workplace mental health, see the World Health Organization’s Mental Health at Work fact sheet.
Anxiety’s Physical Sequelae on College Campuses
Young Adults at Risk for Early-Onset Chronic Disease
- Emerging Hypertension: College students with persistent anxiety exhibit early markers of cardiovascular risk—elevated blood pressure and pulse wave velocity.
- Gastrointestinal Complaints: Over 50% of anxious students report frequent stomach cramps, diarrhea, or reflux, negatively impacting nutrition and academic performance.
- Poor Sleep and Obesity: Chronic anxiety disrupts sleep architecture, leading to both fatigue and altered appetite hormones—contributing to unhealthy weight gain.
Long-Term Concern: Patterns established in early adulthood often persist, setting the stage for chronic illness decades later. The American College Health Association annual report offers extensive data.
Strategies to Counteract Physical Aftereffects
Organizational and Institutional Interventions
- Holistic Wellbeing Programs:
- Incorporate physical health screenings—blood pressure checks, BMI assessments, and glucose monitoring—into mental health initiatives.
- Offer on-site fitness facilities, ergonomic assessments, and nutritional counseling alongside counseling services.
- Stress-Reduction Infrastructure:
- Design “quiet pods” and mindfulness rooms.
- Implement mandatory breaks and limit prolonged screen time.
- Educational Campaigns:
- Raise awareness of anxiety’s physical consequences through workshops and informational materials.
- Train leaders to recognize early signs of physical stress—such as frequent headaches or gastrointestinal complaints—and facilitate timely support.
For workplace program examples, explore Mental Health America’s workplace resources.
Individual Self-Care Practices
- Regular Exercise: Aerobic activity reduces cortisol levels and improves cardiovascular resilience. A routine of 150 minutes per week can lower anxiety symptoms by up to 30%.
- Mind–Body Techniques: Practices like yoga and progressive muscle relaxation attenuate HPA axis activation and reduce pain sensitivity. The National Center for Complementary and Integrative Health details effective mind–body practices.
- Structured Sleep Hygiene: Consistent sleep schedules and pre-sleep routines support hormonal balance, reducing metabolic disruption.
- Balanced Nutrition: Diets rich in omega-3 fatty acids, fiber, and antioxidants combat inflammation and support gut health.
Conclusion
The escalating anxiety epidemic in corporate offices and college campuses no longer confines its damage to the psyche. Chronic stress now manifests as hypertension, gastrointestinal disorders, immune dysfunction, chronic pain, and metabolic syndrome—foreshadowing lifelong health burdens. Addressing anxiety’s physical aftereffects demands a paradigm shift: from siloed mental health services to integrated wellbeing ecosystems that fortify both mind and body. By embedding comprehensive health screenings, fostering restorative work and study environments, and empowering individuals with holistic coping tools, organizations and institutions can break the cycle of chronic disease and pave the way for sustainable health.
External Resources for Further Reading
- Anxiety and Depression Association of America: https://adaa.org/understanding-anxiety
- National Institute of Mental Health: https://www.nimh.nih.gov/health/topics/anxiety-disorders
- Centers for Disease Control and Prevention (Stress & Coping): https://www.cdc.gov/mentalhealth/stress-coping/index.html
- World Health Organization: Mental Health at Work – https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work
- American Psychological Association: Allostatic Load – https://www.apa.org/topics/stress/allostatic-load
- American College Health Association: https://www.acha.org/
- Mayo Clinic: Fibromyalgia – https://www.mayoclinic.org/diseases-conditions/fibromyalgia/symptoms-causes/syc-20354780