The COVID-19 pandemic triggered a global mental health crisis, with anxiety and depression rates doubling worldwide. Social isolation, economic uncertainty, and disrupted healthcare systems created a perfect storm that continues to impact mental well-being years later, particularly among women, young people, and vulnerable populations.
Introduction
While the world focused on containing the spread of COVID-19, a parallel pandemic was silently unfolding—one that affected the mind rather than the body. The psychological toll of the pandemic has proven to be one of its most enduring legacies, fundamentally altering the mental health landscape across the globe. From the initial lockdowns in early 2020 to the ongoing post-pandemic recovery, the crisis has exposed the fragility of our collective mental well-being and highlighted the urgent need for comprehensive mental health infrastructure. This examination explores the magnitude of COVID-19’s impact on mental health, the specific populations most affected, and the emerging trends as society attempts to heal from this unprecedented global trauma.
The Scale of the Mental Health Crisis
Global Statistics: A Worldwide Emergency
The World Health Organization’s landmark assessment in March 2022 revealed the staggering scope of the crisis: global prevalence of anxiety and depression increased by a massive 25% in the first year of the pandemic alone. This represents one of the most significant mental health disruptions in recorded history, affecting hundreds of millions of people worldwide.
More detailed analysis published in The Lancet revealed even more concerning figures, showing a 27.6% increase in cases of major depressive disorders and a 25.6% increase in anxiety disorders globally throughout 2020. To put this in perspective, these increases translate to approximately 76 million additional cases of anxiety disorders and 53 million additional cases of major depressive disorders worldwide.
The American Experience: A Mental Health Emergency
In the United States, the crisis was particularly acute. Boston College researchers tracking mental health throughout the pandemic found that anxiety rates skyrocketed to 50% and depression to 44% by November 2020—representing rates six times higher than 2019 levels. Among young adults aged 18-29, the statistics were even more alarming, with anxiety and depression rates reaching 65% and 61% respectively.
The Kaiser Family Foundation’s ongoing research revealed that by early 2021, approximately four in ten adults were reporting symptoms consistent with anxiety and depression, before declining slightly to three in ten adults as the pandemic continued but remaining well above pre-pandemic levels. This persistent elevation indicates the enduring nature of pandemic-related mental health impacts.
Children and Adolescents: The Most Vulnerable Population
Perhaps the most heartbreaking aspect of the mental health pandemic has been its impact on children and young people. A comprehensive meta-analysis of 29 studies involving 80,879 youth globally found that 25.2% experienced clinically elevated depression symptoms and 20.5% experienced clinically elevated anxiety symptoms during COVID-19. This represents a doubling of pre-pandemic rates, which stood at 12.9% for depression and 11.6% for anxiety.
The analysis revealed several disturbing trends:
- One in four youth globally were experiencing clinically elevated depression symptoms
- One in five youth were experiencing clinically elevated anxiety symptoms
- Rates increased as the pandemic progressed, suggesting a cumulative impact of ongoing stress
- Female adolescents were disproportionately affected, with the gender gap widening significantly
The Mechanisms of Mental Health Deterioration
Social Isolation: The Primary Driver
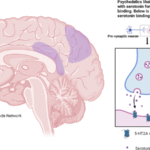
The unprecedented social isolation imposed by lockdowns and distancing measures emerged as the primary driver of mental health deterioration. A comprehensive study published in Nature revealed the profound neurobiological consequences of mass social isolation, documenting elevated levels of anxiety and depression, deterioration of mental health, changes in diet, increased suicidal ideation, reduced physical activity, and higher levels of experienced loneliness.
Research showed that rates of loneliness were twice as high among people who met clinical criteria for depression, anxiety, and post-traumatic stress disorder compared to the general population. The study found that individuals who were self-isolating alone and unemployed experienced the highest prevalence of loneliness, while those who were married or living with a partner showed greater resilience.
Economic Devastation and Mental Health
The economic impact of the pandemic created a secondary wave of mental health challenges. Individuals experiencing household job loss were significantly more likely than their counterparts to report symptoms of anxiety and/or depression (53% vs. 30%) in February 2023. The relationship between unemployment and mental health deterioration during the pandemic was particularly stark, with financial stress serving as a major predictor of psychological distress.
Healthcare System Disruption
The pandemic created severe disruptions to mental health services at precisely the moment when they were needed most. For much of the pandemic, mental health services were among the most disrupted of all essential health services reported by WHO Member States. Many countries reported major disruptions in life-saving services for mental health, including suicide prevention programs, leaving huge gaps in care for those who needed it most.
Demographic Disparities: Who Suffered Most?
Women: Bearing the Brunt of the Crisis
Women experienced disproportionately higher rates of mental health problems during the pandemic. Symptoms of anxiety and/or depression were elevated among women (36%) compared to men (28%) in February 2023. Research consistently showed that compared to men, women experienced more overall distress and higher levels of panic, depression, emotional disturbances, and concerns about contracting COVID-19 and about the safety of their family.
The gender disparity was particularly pronounced among adolescents. The gap in the share of adolescent females and males reporting feelings of hopelessness and sadness widened dramatically from 2019 (47% vs. 27%, respectively) to 2021 (57% vs. 29%, respectively).
Young Adults: A Generation in Crisis
Young adults emerged as the most psychologically vulnerable demographic. Fifty percent of young adults (ages 18-24) reported anxiety and depression symptoms in 2023, making them significantly more likely than older adults to experience mental health symptoms. This age group faced unique pandemic-related challenges including university closures, transitioning to remote work, loss of income or employment, and disrupted social developmental milestones.
Vulnerable Populations: Compounded Trauma
The pandemic exacerbated existing mental health disparities across racial, ethnic, and socioeconomic lines. Rates of mental health disorders were highest among young, less-educated, single parent, female, Black and Hispanic respondents. These disparities widened over time, indicating that the pandemic’s mental health impact was not equally distributed across society.
People experiencing homelessness faced particularly severe challenges. Research found that social isolation worsened mental health conditions and contributed to increased substance use and overdoses among this population. For individuals with serious mental illness experiencing homelessness, feelings of paranoia intensified with the onset of COVID-19, with many believing the pandemic was “targeted against them.”
Long-Term Consequences and Post-Pandemic Trends
The Persistence of Mental Health Impacts
Contrary to initial hopes that mental health would rapidly rebound as pandemic restrictions lifted, research reveals persistent and in some cases worsening mental health outcomes. A study of Finnish adolescents comparing pre-pandemic (2018) to post-pandemic (2022) mental health found they reported more mental health problems after the peak of the pandemic, with 99% reporting feelings of loneliness.
Long COVID and Mental Health Comorbidity
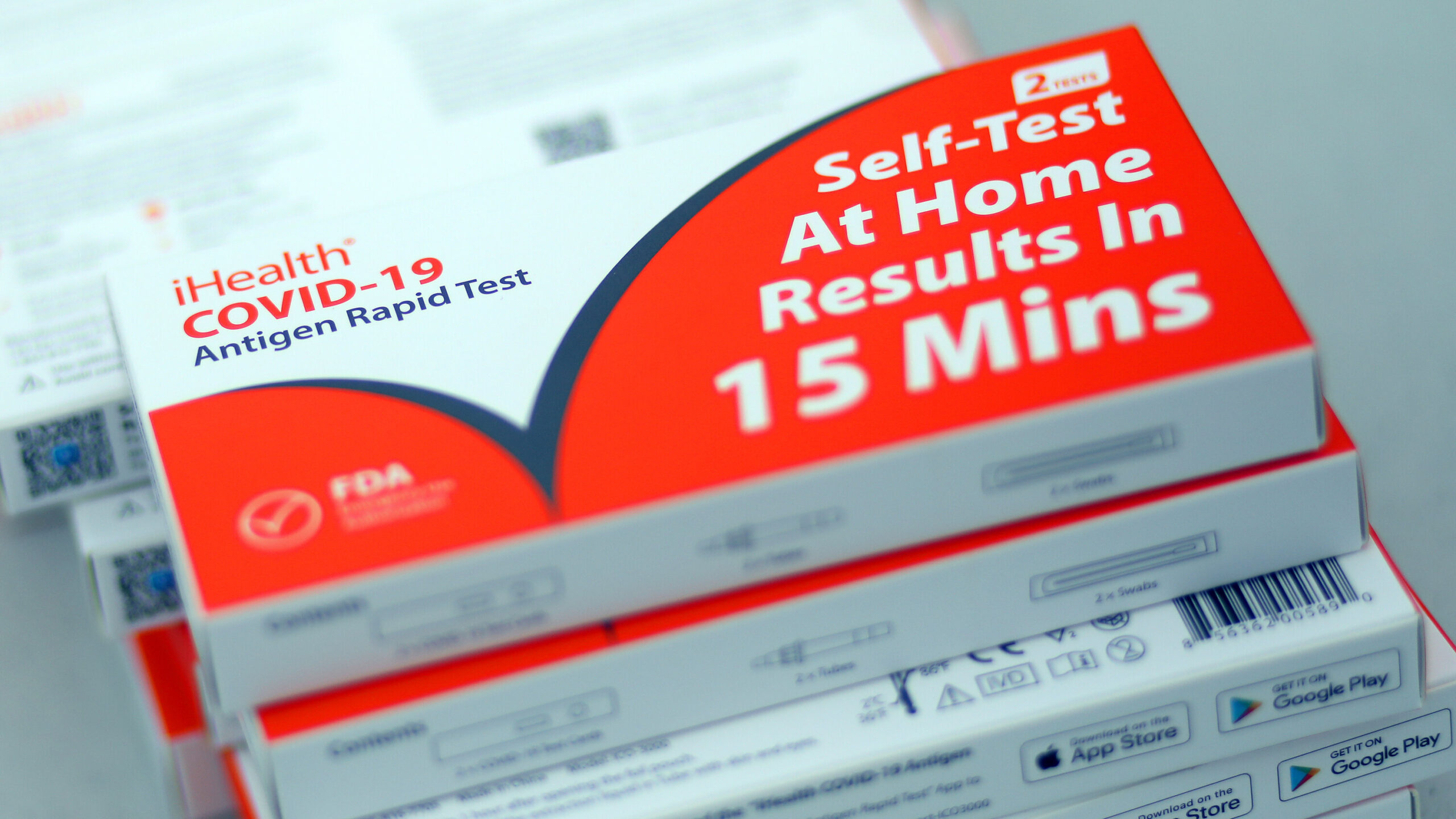
The emergence of Long COVID has created an additional layer of mental health complexity. An estimated 28% of U.S. adults who have had acute COVID-19 infections report experiencing Long COVID at some point. Among the neuropsychiatric manifestations most frequently associated with Long COVID are depression, anxiety, post-traumatic stress disorder, sleep disturbances, fatigue, and cognitive deficits.
Dr. Jordan Anderson, a neuropsychiatrist at Oregon Health and Science University, reports that “depression is the most prominent symptom we see” in Long COVID patients, along with significant rates of anxiety, panic attacks, and PTSD. Studies show that up to 56% of COVID-19 survivors scored in the pathological range for at least one clinical dimension at one month post-infection, with 35.8% still showing pathological scores at three months.
Educational Impact and Recovery Challenges
School closures had profound and lasting effects on children’s mental health. A longitudinal study found that in-person school attendance was the most protective factor against elevated mental health symptoms during the pandemic. Research from Kenya showed that out-of-school adolescents exhibited significantly higher prevalence of anxiety and depression compared to those who returned to school after reopening.
Children with neurodevelopment disorders, including ADHD and Autism Spectrum Disorder, showed particular vulnerabilities, with interrupted services and delayed diagnoses escalating the risk of crisis, including suicidal behaviour.
Positive Adaptations and Resilience
Despite the overwhelming challenges, some research revealed positive adaptations and resilience. A study across 22 European and Central Asian countries found that 51% of adolescents perceived pandemic measures as neutral and 31% as positive, with only 18% viewing them negatively. Some youth reported that isolation periods allowed for positive life outcomes relating to personal health and fostered stronger senses of empathy, compassion, and gratitude.
Interestingly, some adolescents in Canada reported getting more than the recommended amount of sleep during the pandemic and were less tired during the day due to delayed schedules that better matched their natural circadian rhythms.
The Path Forward: Recovery and Resilience
Immediate Interventions Needed
The mental health crisis requires immediate, comprehensive intervention across multiple sectors:
Healthcare System Strengthening: Expansion of telepsychiatry services, which proved effective during the pandemic, can provide cost-effective access to mental health care. Integration of mental health screening into primary care settings is essential for early identification and intervention.
Educational Support: Schools must prioritize mental health support, with research showing that positive student-teacher relationships and peer support are crucial protective factors. Programs focusing on health literacy and emotional regulation should be integrated into curricula.
Community-Based Services: Investment in community mental health services, particularly for vulnerable populations, is critical. Support for volunteer and community programs that reduce loneliness and foster social connections must be maintained and expanded.
Addressing Systemic Issues
Long-term recovery requires addressing the systemic issues that exacerbated the mental health crisis:
Economic Support: Policies addressing income inequality, job security, and financial stability are essential for mental health recovery. The strong correlation between financial stress and mental health problems demands comprehensive economic interventions.
Social Infrastructure: Investment in social infrastructure that prevents isolation and builds community connections is crucial. This includes accessible public spaces, community centers, and programs that foster social cohesion.
Mental Health Parity: Ensuring that mental health treatment is covered by insurance plans and integrated into healthcare benefit packages is essential for addressing the treatment gap.
Preparing for Future Crises
The COVID-19 pandemic has provided valuable lessons for managing mental health during public health emergencies:
Early Warning Systems: Development of systems to monitor and respond to population mental health trends during crises is essential.
Flexible Service Delivery: The success of telepsychiatry and remote mental health services demonstrates the need for flexible, multi-modal service delivery systems.
Vulnerable Population Focus: Future emergency responses must prioritize the mental health needs of vulnerable populations from the outset rather than as an afterthought.
Conclusion
The COVID-19 pandemic’s impact on global mental health represents one of the most significant public health challenges of the 21st century. With anxiety and depression rates doubling worldwide, an entire generation of children and young people affected, and persistent mental health challenges continuing years after initial lockdowns, the crisis demands sustained, comprehensive intervention.
The pandemic exposed fundamental weaknesses in global mental health infrastructure while also demonstrating remarkable adaptability and resilience in service delivery. The success of telepsychiatry, the critical importance of social connections, and the disproportionate impact on vulnerable populations provide crucial insights for building more robust, equitable mental health systems.
As we move forward in the post-pandemic era, the mental health crisis requires the same level of urgency, resources, and coordinated response that was mobilized for the physical health emergency. The psychological wounds of the pandemic may prove to be its most enduring legacy, but with appropriate intervention, they also represent an opportunity to build better, more resilient mental health systems that can serve society for generations to come.
The path to recovery is long and complex, but the research clearly shows that early intervention, sustained support, and systemic change can help heal the psychological trauma of the pandemic and build resilience for future challenges.
Trusted Resources for Further Reading:
- World Health Organization: COVID-19 pandemic triggers 25% increase in anxiety and depression – https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide
- Kaiser Family Foundation: Mental Health and Substance Use Implications of COVID-19 – https://www.kff.org/mental-health/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/
- Nature: Social isolation and the brain in the pandemic era – https://www.nature.com/articles/s41562-022-01453-0
- JAMA Pediatrics: Global Prevalence of Child and Adolescent Mental Health During COVID-19 – https://jamanetwork.com/journals/jamapediatrics/fullarticle/2782796