Depression is escalating worldwide, with women disproportionately affected. Beyond its profound mental health impact, chronic depression precipitates serious physical illnesses—cardiovascular disease, metabolic syndrome, immune dysfunction, and chronic pain—trapping individuals in a vicious cycle that undermines recovery.
Introduction
Depression—once stigmatized and underrecognized—is now acknowledged as a leading cause of disability globally. Intensified by social upheavals, economic instability, and digital overload, its prevalence has surged, exacting not only psychological but also severe physiological costs. This comprehensive blog examines:
- Trends driving the global increase in depression
- Gender disparities and underlying causes
- Long-term physical health consequences
- How depression erodes physical resilience and perpetuates its own cycle
- Evidence-based interventions
Credible data from the World Health Organization (WHO), Global Burden of Disease (GBD) studies, the U.S. Centers for Disease Control and Prevention (CDC), and peer-reviewed research form the backbone of this analysis.
The Rising Tide: Global Depression Trends
Prevalence Over Time
- According to the GBD 2019 analysis, documented cases of depressive disorders climbed from 182 million in 1990 to 290 million in 2019—a 59% absolute increase (nature).
- The WHO estimates 5% of adults worldwide suffer from depression, encompassing 4% of men and 6% of women (who).
- In the U.S. between August 2021 and August 2023, the two-week prevalence of depression among individuals aged 12 and older was 13.1% (cdc).
Why Depression Is Climbing
Several interrelated factors fuel the upward trajectory of depression:
Modernisation and Lifestyle Shifts
- Sedentary Behaviour & Poor Diet: Modern industrial lifestyles promote inactivity and processed-food consumption, both linked to increased depression risk (pmc.ncbi.nlm.nih).
- Sleep Deprivation & Light Pollution: Reduced natural light exposure and erratic sleep–wake cycles disregulate circadian rhythms and mood.
- Social Isolation & Loneliness: Declining social capital and greater societal inequality foster feelings of alienation, a potent depresso-genic factor (pmc.ncbi.nlm.nih)
Technological Overload
- Digital Media Multitasking: Constant notifications and information bombardment impair attention and exacerbate rumination—a core feature of depression.
- Social Comparison: Curated online lives fuel unrealistic expectations, self-criticism, and diminished self-worth.
Socioeconomic Stressors
- Economic Instability: Job insecurity, income inequality, and skyrocketing living costs heighten financial anxiety and depressive symptoms.
- Global Crises: COVID-19 triggered a 25% global rise in depression prevalence in 2020, driven by isolation, health fears, bereavement, and economic uncertainty (who).
Increased Detection and Reduced Stigma
- Improved mental health awareness campaigns and greater access to screening have led to higher diagnostic rates, partially accounting for the observed rise.
Gender Disparities in Depression
Comparative Prevalence
- The WHO reports adults with depression: 4% of men vs. 6% of women (who).
- U.S. data show current prevalence: 10.1% in males and 16.0% in females (cdc).
- GBD 2019 incidence: 110 million cases in men vs. 180 million in women, with women accruing nearly 28.7 million versus 18.2 million in men (nature).
Why Women Are More Affected
- Hormonal Fluctuations:
Estrogen and progesterone modulate neurotransmitter systems; menstrual cycles, postpartum changes, and menopause increase vulnerability. - Psychosocial Pressures:
Women often juggle professional roles with disproportionate caregiving and domestic responsibilities, amplifying stress. - Higher Rates of Trauma Exposure:
Women experience greater incidence of domestic violence and sexual assault, potent precipitants of depression. - Help-Seeking Behavior:
Women are more likely to report symptoms and seek care, partly explaining higher diagnosed prevalence.
Long-Term Physical Health Consequences of Chronic Depression
Depression induces persistent physiological alterations—many of which directly contribute to chronic disease.
Cardiovascular Disease
- Increased Risk: Major depression is associated with a 60% higher likelihood of coronary artery disease and heart failure.
- Mechanisms: Elevated cortisol and catecholamines accelerate atherosclerosis via endothelial dysfunction; autonomic imbalance elevates resting heart rate and blood pressure.
Metabolic Syndrome and Diabetes
- Insulin Resistance: Chronic stress hormones impair insulin sensitivity, raising fasting glucose and HbA1c.
- Obesity: Depressive symptoms reduce physical activity and promote unhealthy eating, increasing visceral adiposity. Individuals with depression have a 30% greater risk of developing type 2 diabetes.
Immune Disregulation
- Proinflammatory State: Depression elevates cytokines (IL-6, TNF-α), contributing to systemic inflammation.
- Infection Susceptibility: Impaired lymphocyte proliferation and NK cell function result in higher rates of infections and slower recovery.
Chronic Pain and Musculoskeletal Disorders
- Fibromyalgia & Widespread Pain: Central sensitization—heightened pain processing in the CNS—is exacerbated by depression, leading to chronic pain syndromes.
- Back Pain and Migraines: Depressed individuals report 40% higher incidence of chronic back pain and tension-type headaches.
Gastrointestinal Disorders
- Irritable Bowel Syndrome (IBS): Depression disrupts gut–brain axis signaling; up to 60% of IBS patients exhibit comorbid major depression.
- Peptic Ulcers: Stress hormones weaken gastric mucosal defenses, increasing ulcer risk.
The Vicious Cycle: How Depression Undermines Physical Recovery
Behavioral Pathways
- Reduced Self-Care: Apathy, fatigue, and cognitive impairment diminish adherence to medical regimens, healthy diets, and exercise.
- Sleep Disturbances: Insomnia and hypersomnia impair restorative processes essential for immunity, cognition, and tissue repair.
Biological Feedback Loops
- Neuroendocrine Synchronization: Persistent HPA-axis hyperactivity perpetuates cortisol elevation, further damaging cardiovascular, metabolic, and immune systems.
- Neuroplastic Changes: Chronic depression remodels brain circuits (hippocampus, prefrontal cortex), impairing stress regulation and resilience.
As physical health deteriorates, functional impairments and pain amplify psychological distress, deepening depressive symptoms and making recovery increasingly elusive.
Breaking the Cycle: Integrated Prevention and Treatment
Holistic Healthcare Models
- Collaborative Care: Embedding mental health specialists in primary care enables simultaneous management of depression and chronic physical illnesses.
- Regular Screening: Routine assessment of depressive symptoms in patients with cardiovascular disease, diabetes, and autoimmune disorders.
Lifestyle Interventions
- Exercise Prescription: Aerobic and resistance training at least 150 minutes/week reduces depressive symptoms by 30–40%, while improving cardiovascular and metabolic health.
- Nutrition Optimization: Diets rich in omega-3 fatty acids, whole grains, lean proteins, fruits, and vegetables mitigate inflammation and support neurotransmitter synthesis.
- Sleep Hygiene: Cognitive-behavioral therapy for insomnia (CBT-I) restores circadian balance and enhances mood regulation.
Psychotherapeutic Approaches
- Cognitive-Behavioral Therapy (CBT): Targets negative thought patterns and promotes behavioral activation.
- Mindfulness-Based Stress Reduction (MBSR): Lowers cortisol, reduces inflammatory markers, and improves autonomic function.
- Interpersonal Therapy (IPT): Addresses relationship challenges and social support deficits—vital for both genders but especially beneficial for women experiencing role overload.
Pharmacological Management
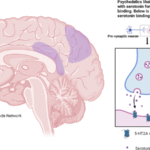
- Antidepressants: SSRIs and SNRIs improve mood and display ancillary benefits, such as anti-inflammatory effects; careful monitoring is needed for metabolic side effects.
- Adjunctive Therapies: Anti-inflammatories and metabolic agents (e.g., metformin) may counteract depression-related physiological dysregulation.
Conclusion
The global escalation of depression—particularly among women—poses a dual threat: profound psychological suffering and a cascade of debilitating physical illnesses. By comprehensively addressing both mental and physical dimensions through integrated care models, lifestyle modifications, and targeted therapies, we can disrupt the vicious cycle that renders depression so intractable. Collective action—from policymakers funding mental health infrastructure to clinicians adopting holistic practices and individuals engaging in self-care—remains paramount to reversing this crisis and restoring health in body and mind.
External Resources for further research
- World Health Organization: Depressive Disorder Fact Sheet – https://www.who.int/news-room/fact-sheets/detail/depression
- Centers for Disease Control and Prevention: Depression Prevalence Data – https://www.cdc.gov/nchs/products/databriefs/db527.htm
- Global Burden of Disease Study 2019 – https://www.nature.com/articles/s41598-024-62381-9
- Brandon H. Hidaka: Depression as a Disease of Modernity – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3330161/
- NIH: Stress and Immunity Research – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3966022/