Imagine waking up one morning and suddenly the world doesn’t make sense anymore. The voices of your family sound different, shadows seem to move on their own, and you start hearing conversations that others can’t hear. This is the frightening reality that millions of people face when schizophrenia enters their lives. Far from the Hollywood stereotypes of “split personalities,” schizophrenia is a complex brain condition that fundamentally changes how someone experiences reality, relationships, and their place in the world.
What is Schizophrenia and How Do We Recognize It?
Schizophrenia is a brain disorder that affects how people think, feel, and perceive the world around them. It’s not about having multiple personalities – that’s a completely different condition. Instead, schizophrenia involves a break from reality that can be terrifying for both the person experiencing it and their loved ones.
The condition typically emerges during a crucial time in life – the late teens to mid-twenties – when young people are supposed to be launching their careers, forming relationships, and discovering who they are. This timing makes schizophrenia particularly devastating, as it strikes just when people are building their adult lives.
The Challenge of Getting a Diagnosis
Unlike a broken bone that shows up clearly on an X-ray, diagnosing schizophrenia requires careful observation over time. There’s no blood test or brain scan that can definitively say “this person has schizophrenia.” Instead, mental health professionals must piece together a complex puzzle of symptoms, behaviors, and experiences.
The Diagnostic Criteria: To receive a schizophrenia diagnosis, a person must experience at least two of these symptoms for a significant portion of time during one month, with some level of disturbance lasting at least six months:
- Delusions: False beliefs that feel absolutely real, like thinking the government is monitoring your thoughts
- Hallucinations: Usually hearing voices that others can’t hear, though it can involve any of the senses
- Disorganized speech: Jumping between unrelated topics or speaking in ways that don’t make logical sense
- Disorganized or catatonic behavior: Moving in strange ways or becoming completely still
- Negative symptoms: Losing the ability to function normally, like neglecting hygiene or withdrawing from social contact
Why Diagnosis Takes Time: Doctors need to rule out other conditions that can mimic schizophrenia, including drug use, brain tumors, or other psychiatric conditions. They also need to see how symptoms develop over time, as many conditions can cause temporary psychotic episodes.
The Phases of Schizophrenia
Schizophrenia typically unfolds in three distinct phases:
The Prodromal Phase: This is like the warning tremor before an earthquake. About 75% of people with schizophrenia experience this phase, which can last weeks to several years. During this time, subtle changes begin:
- Social withdrawal and losing interest in activities
- Difficulty concentrating or thinking clearly
- Changes in sleep patterns and personal hygiene
- Mild depression, anxiety, or mood swings
- Unusual beliefs or slight paranoia
The Active Phase: This is when full psychotic symptoms appear – hallucinations, delusions, and severely disorganized thinking. It’s often when families realize something is seriously wrong and seek help.
The Residual Phase: With treatment, acute symptoms typically improve, but some challenges may remain, such as difficulty concentrating or reduced motivation.
How Schizophrenia Rewrites the Brain’s Blueprint
Understanding what happens inside the brain helps explain why schizophrenia is such a challenging condition. Research shows that schizophrenia involves significant changes to brain structure and function.
The Neurodevelopmental Story
Scientists now understand schizophrenia as a neurodevelopmental disorder. This means the roots of the condition may begin forming much earlier than when symptoms appear – possibly even before birth. Think of it like a software bug that doesn’t cause problems until the program becomes more complex.
The Two-Hit Model: Researchers propose that schizophrenia develops through a “two-hit” process:
- First Hit: Early developmental problems (genetic factors, infections during pregnancy, or complications at birth) create vulnerabilities in brain development
- Second Hit: During adolescence, normal brain changes (like pruning unnecessary connections) can trigger the emergence of symptoms in those who are already vulnerable
Brain Changes That Matter
Gray Matter Loss: Multiple studies show that people with schizophrenia have reduced gray matter – the brain tissue packed with neurons that do the actual thinking. This loss is particularly noticeable in areas responsible for:
- Prefrontal cortex: Decision-making and planning
- Temporal lobes: Memory and language processing
- Hippocampus: Learning and memory formation
White Matter Disruption: The brain’s “wiring” – white matter that connects different regions – also becomes damaged. Using special brain imaging, scientists can see that the pathways connecting different brain areas become less efficient, like having poor internet connections between computers.
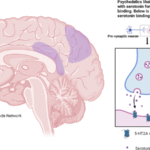
Chemical Imbalances: Two brain chemicals are particularly affected:
- Dopamine: Too much activity in some areas (causing hallucinations and delusions) and too little in others (causing motivation problems)
- Glutamate: Reduced function of this important neurotransmitter affects thinking and perception
What This Means in Real Life
These brain changes aren’t just medical statistics – they translate into real challenges:
Cognitive Problems: Many people with schizophrenia struggle with what scientists call “cognitive symptoms” – problems with attention, memory, and thinking that can be more disabling than hallucinations. Imagine trying to work when you can’t concentrate for more than a few minutes or can’t remember instructions.
Social Cognition Difficulties: The brain changes affect the ability to understand social cues, read facial expressions, or interpret tone of voice. This makes social interactions feel like trying to navigate a foreign culture without understanding the language.
The Social Earthquake: How Schizophrenia Destroys Relationships
Perhaps the most heartbreaking aspect of schizophrenia is how it can isolate someone from the people they love most. The condition doesn’t just affect the person diagnosed – it sends shockwaves through their entire social network.
The Communication Breakdown
During Psychotic Episodes: When someone is experiencing active symptoms, communication becomes nearly impossible. They might respond to voices others can’t hear, believe things that aren’t true, or speak in ways that don’t make sense. Family members often describe feeling like they’re talking to a stranger.
The Trust Erosion: Paranoid thoughts can make someone suspicious of even their closest family members. A mother might become convinced her daughter is trying to poison her, or a husband might believe his wife is part of a conspiracy against him. These delusions feel absolutely real to the person experiencing them.
Emotional Distance: Negative symptoms can make someone seem emotionally “flat” or unresponsive. They might not react to good news, seem uninterested in activities they used to love, or appear not to care about relationships. This isn’t a choice – it’s a symptom of the illness.
The Ripple Effects on Family
Living with schizophrenia affects everyone in the household:
Role Reversal: Children might become caregivers for parents, or spouses might take on responsibilities their partner can no longer handle. These role changes can create stress and resentment.
Emotional Exhaustion: Family members often experience their own mental health challenges, including depression, anxiety, and burnout from constant caregiving.
Social Isolation: Stigma around mental illness can cause families to withdraw from their own social circles, leading to isolation and reduced support.
The Workplace Challenge
Employment becomes a major struggle for people with schizophrenia. The statistics are sobering: unemployment rates can reach 80-90%, even though about 90% of people with schizophrenia want to work.
The Barriers Are Real:
- Cognitive challenges: Difficulty concentrating, remembering instructions, or processing information quickly
- Social difficulties: Problems reading workplace social cues or interacting with colleagues
- Symptom management: Dealing with medication side effects during work hours
- Stigma: Employer discrimination and fear of disclosure
The Performance Puzzle: Even when someone finds work, maintaining consistent performance can be challenging. Good days might be followed by difficult days when symptoms are more prominent, creating a pattern that employers might misinterpret as unreliability.
The Friendship Casualty
Friendships often become casualties of schizophrenia:
Social Withdrawal: During the prodromal phase, people often pull away from friends before anyone understands why. This withdrawal intensifies during active phases of the illness.
Stigma and Fear: Friends might not understand the condition and may distance themselves out of fear or discomfort. The media’s portrayal of schizophrenia as violent (despite most people with the condition being more likely to be victims than perpetrators) doesn’t help.
Communication Challenges: The thinking and speech problems that come with schizophrenia can make social interactions awkward or difficult to maintain.
The Daily Reality: Living with Schizophrenia
Understanding the day-to-day reality of living with schizophrenia helps us grasp why it’s such a challenging condition. Here’s what a typical day might look like:
The Morning Struggle
Someone with schizophrenia might wake up to voices commenting on their every move. The medication that helps control symptoms might cause drowsiness, making it hard to get up. Simple decisions like what to wear can become overwhelming when thinking is clouded.
Social Interactions Feel Different
Every conversation becomes a minefield. Is that person really talking about them, or is it paranoia? Are the voices they’re hearing real or not? Social situations that used to feel natural now require constant mental energy to navigate.
Work and School Challenges
Concentrating on tasks becomes difficult when your brain is dealing with internal noise. Following complex instructions might be impossible when working memory isn’t functioning well. Colleagues’ casual conversations might feel threatening when paranoid thoughts are active.
The Medication Balancing Act
Antipsychotic medications can be lifesaving, but they often come with side effects like weight gain, drowsiness, or movement problems. Finding the right medication at the right dose is often a long process of trial and adjustment.
Hope and Healing: Coping Strategies That Work
Despite these challenges, recovery and meaningful life are possible with schizophrenia. The key is understanding that “recovery” doesn’t necessarily mean being symptom-free – it means learning to manage the condition and building a satisfying life.
Medication: The Foundation
Antipsychotic medications remain the cornerstone of treatment. These medications work by adjusting brain chemistry, particularly dopamine levels. While they don’t cure schizophrenia, they can significantly reduce symptoms and prevent relapses.
The Reality: Finding the right medication often takes time. What works for one person might not work for another, and side effects can be challenging. However, newer medications often have fewer side effects than older ones.
Therapy: Learning to Cope
Cognitive Behavioral Therapy (CBT) helps people learn to challenge distorted thoughts and develop coping strategies. It’s particularly helpful for managing paranoid thoughts and developing insight into the condition.
Family Therapy can be crucial for healing relationships and teaching everyone how to communicate better. It helps family members understand the condition and learn supportive ways to interact.
Support Groups connect people with others who understand their experiences. This peer support can reduce isolation and provide practical coping tips.
Self-Management Strategies
Stress Management: Since stress can trigger symptoms, learning stress reduction techniques is crucial. This might include meditation, deep breathing exercises, or regular physical activity.
Routine and Structure: Consistent daily routines can provide stability and reduce anxiety. Regular sleep, meals, and activities help create a sense of predictability.
Symptom Monitoring: Learning to recognize early warning signs of symptom increases can help prevent full relapses. Many people keep mood diaries or use apps to track their symptoms.
Healthy Lifestyle: Regular exercise, good nutrition, and avoiding drugs and alcohol can significantly improve outcomes. Sleep is particularly important, as sleep disruption often triggers symptoms.
Building Social Skills
Social Skills Training can help people relearn how to navigate social situations. This might include practicing conversations, learning to read social cues, or developing conflict resolution skills.
Gradual Re-engagement: Starting with small, low-pressure social activities can help build confidence before tackling more challenging social situations.
How to Help Someone with Schizophrenia: A Guide for Family and Friends
Supporting someone with schizophrenia requires patience, understanding, and specific skills. Here’s how you can help:
Education is Your Starting Point
Learn About the Condition: Understanding that schizophrenia is a brain disorder, not a character flaw, helps you respond with compassion rather than frustration. Learn about symptoms, treatments, and what recovery looks like.
Understand the Phases: Knowing the difference between prodromal, active, and residual phases helps you adjust your expectations and support accordingly.
Communication Strategies That Work
Focus on Feelings, Not Facts: When someone is experiencing delusions, don’t argue about what’s real. Instead of saying “That’s not true,” try “That sounds really frightening. How can I help you feel safer?”
Stay Calm and Consistent: During psychotic episodes, your calm presence can be an anchor. Speak slowly, use simple language, and avoid overwhelming them with too much information at once.
Listen Without Judgment: Sometimes the most helpful thing you can do is simply listen. Validate their feelings even if you can’t validate their experiences: “I can see this is really distressing for you.”
Practical Support
Help with Daily Tasks: During difficult periods, basic activities like grocery shopping, cooking, or managing appointments might become overwhelming. Offer specific help: “I’m going to the store. What do you need?”
Medication Support: Help them remember to take medications and attend appointments, but avoid being pushy or controlling about it. Work with them to develop systems that work.
Crisis Planning: During stable periods, work together to create a plan for what to do if symptoms worsen. Include emergency contacts, preferred hospitals, and strategies that have helped before.
Building Their Support Network
Encourage Professional Help: Gently support their engagement with mental health services without being demanding. Offer to drive to appointments or sit in waiting rooms for moral support.
Connect with Others: Help them find support groups or peer support programs where they can connect with others who understand their experiences.
Maintain Social Connections: Encourage gentle social activities without being overwhelming. Sometimes this means accepting their need for space while staying consistently available.
Supporting Treatment Adherence
Understand Medication Challenges: People often stop taking medication when they feel better or when side effects are bothersome. Help them work with their doctor to find solutions rather than just insisting they take their pills.
Celebrate Small Victories: Recovery isn’t linear. Acknowledge progress, even when it’s small. Taking medication consistently, attending therapy, or engaging in social activities are all worth celebrating.
What NOT to Do
Avoid These Responses:
- “You’re just being dramatic”
- “Snap out of it”
- “Everyone hears voices sometimes”
- “You’re fine when you take your medication”
Don’t Take Things Personally: During psychotic episodes, your loved one might say hurtful things or accuse you of being part of conspiracies. Remember that the illness is talking, not the person you love.
Avoid Enabling: While being supportive, don’t make excuses for behaviors that could be dangerous or consistently allow the illness to be used as an excuse for avoiding all responsibilities.
Taking Care of Yourself
Set Boundaries: Supporting someone with schizophrenia can be emotionally draining. It’s okay to need breaks and to have your own life and interests.
Get Your Own Support: Consider joining family support groups or seeking counseling for yourself. You can’t pour from an empty cup.
Maintain Perspective: Remember that you can’t cure your loved one or control their choices. Your role is to offer support, not to fix everything.
Creating a Supportive Environment
Reduce Stress: High-emotion, high-conflict environments can worsen symptoms. Work on creating a calm, predictable home environment.
Structure and Routine: Help establish consistent daily routines without being rigid. Predictability can reduce anxiety and provide stability.
Encourage Independence: While offering support, also encourage independence and decision-making when the person is stable. The goal is to help them live as independently as possible.
The Path Forward: Hope in the Darkness
Schizophrenia is undeniably a serious and challenging condition, but it’s important to remember that it’s not a death sentence for dreams and relationships. With proper treatment, support, and understanding, many people with schizophrenia go on to live meaningful, productive lives.
Recovery is Possible
Research shows that about one-third of people with schizophrenia recover significantly, another third have periodic episodes with good functioning between them, and the final third have more persistent symptoms but can still live fulfilling lives with proper support.
The Importance of Early Intervention
The earlier someone gets help, the better their long-term outcomes tend to be. This is why recognizing prodromal symptoms and seeking help quickly is so important.
Breaking Down Stigma
Perhaps the biggest barrier to recovery isn’t the symptoms themselves, but the stigma that surrounds schizophrenia. When we educate ourselves and others, treat people with dignity and respect, and recognize their humanity beyond their diagnosis, we create environments where recovery is more possible.
Building Community
Recovery rarely happens in isolation. Strong social support, understanding families, supportive employers, and communities that embrace rather than exclude people with mental health conditions all contribute to better outcomes.
The Role of Hope
One of the most important things we can offer someone with schizophrenia is hope – hope that their life isn’t over, that relationships can be rebuilt, that meaningful activity is possible, and that they are valued members of our community.
Conclusion: Beyond the Diagnosis
Schizophrenia may change how someone’s brain works, but it doesn’t change their fundamental worth as a human being. Behind every diagnosis is a person with hopes, dreams, fears, and the same basic needs for connection, purpose, and belonging that we all share.
By understanding schizophrenia as a medical condition rather than a character flaw, by learning how to communicate with compassion rather than fear, and by offering support without taking over, we can help create a world where people with schizophrenia don’t have to face their challenges alone.
The journey with schizophrenia isn’t easy – for the person living with it or for their loved ones. But with patience, proper treatment, understanding, and hope, it’s a journey that can lead to healing, growth, and meaningful connection. Sometimes, the greatest gift we can offer someone struggling with schizophrenia is simply believing in their ability to recover and standing beside them as they find their way back to themselves.
Recovery isn’t about returning to who someone was before – it’s about discovering who they can become despite and because of their challenges. In that discovery, both individuals and communities often find strengths they never knew they had.